SC measles outbreak has gone berserk: 124 cases since Friday, 409 quarantined
A measles outbreak in South Carolina that began in October is now wildly accelerating, doubling in just the past week to a total of 434 cases, with 409 people currently in quarantine.
Amid the outbreak, South Carolina health officials have been providing updates on cases every Tuesday and Friday. On Tuesday, state health officials reported 124 more cases since last Friday, which had 99 new cases since the previous Tuesday. On that day, January 6, officials noted a more modest increase of 26 cases, bringing the outbreak total at that point to 211 cases.
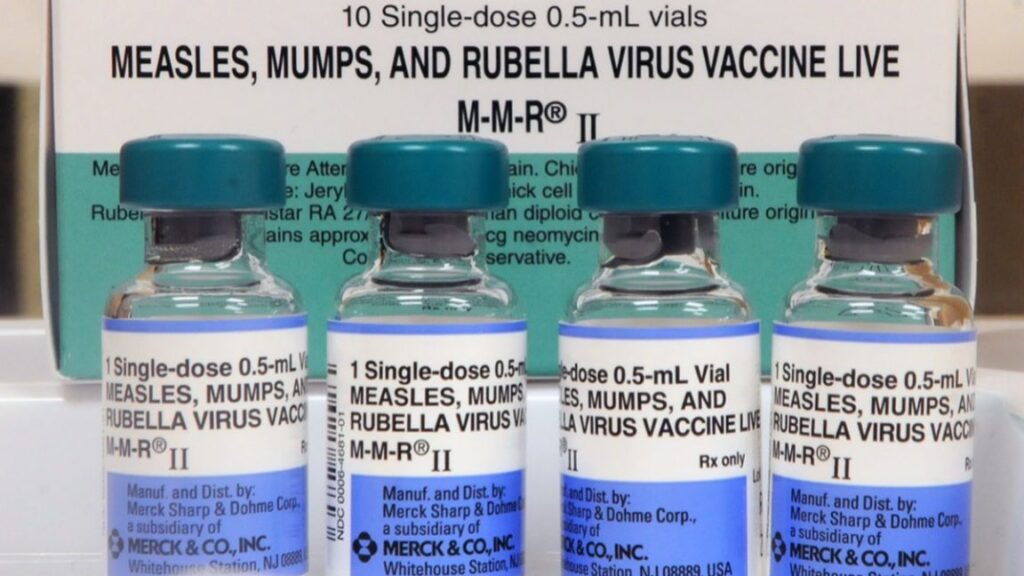
With the 3-month-old outbreak now doubled in just a week, health officials are renewing calls for people to get vaccinated against the highly infectious virus—an effort that has met with little success since October. Still, the health department is activating its mobile health unit to offer free measles-mumps-rubella (MMR) vaccinations, as well as flu vaccinations at two locations today and Thursday in the Spartanburg area, the epicenter of the outbreak.
Officials are also warning that they’re losing the ability to trace cases, and exposures are continuing. Last Friday, someone contagious with measles was in the South Carolina State Museum in Columbia between 1 pm and 5 pm ET. Anyone in the museum during that time and unvaccinated is at risk of contracting the infection. The virus spreads through the air and can linger in a room’s airspace for up to two hours after an infected person has left. Measles is so contagious that up to 90 percent of unvaccinated people exposed will fall ill.
SC measles outbreak has gone berserk: 124 cases since Friday, 409 quarantined Read More »