Measles arrives in Kansas, spreads quickly in undervaccinated counties
On Thursday, the county on the northern border of Stevens, Grant County, also reported three confirmed cases, which were also linked to the first case in Stevens. Grant County is in a much better position to handle the outbreak than its neighbors; its one school district, Ulysses, reported 100 percent vaccination coverage for kindergartners in the 2023–2024 school year.
Outbreak risk
So far, details about the fast-rising cases are scant. The Kansas Department of Health and Environment (KDHE) has not published another press release about the cases since March 13. Ars Technica reached out to KDHE for more information but did not hear back before this story’s publication.
The outlet KWCH 12 News out of Wichita published a story Thursday, when there were just six cases reported in just Grant and Stevens Counties, saying that all six were in unvaccinated people and that no one had been hospitalized. On Friday, KWCH updated the story to note that the case count had increased to 10 and that the health department now considers the situation an outbreak.
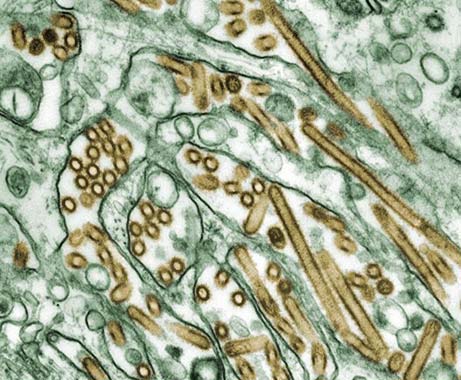
Measles is an extremely infectious virus that can linger in airspace and on surfaces for up to two hours after an infected person has been in an area. Among unvaccinated people exposed to the virus, 90 percent will become infected.
Vaccination rates have slipped nationwide, creating pockets that have lost herd immunity and are vulnerable to fast-spreading, difficult-to-stop outbreaks. In the past, strong vaccination rates prevented such spread, and in 2000, the virus was declared eliminated, meaning there was no continuous spread of the virus over a 12-month period. Experts now fear that the US will lose its elimination status, meaning measles will once again be considered endemic to the country.
So far this year, the Centers for Disease Control and Prevention has documented 378 measles cases as of Thursday, March 20. That figure is already out of date.
On Friday, the Texas health department reported 309 cases in its ongoing outbreak. Forty people have been hospitalized, and one unvaccinated child with no underlying medical conditions has died. The outbreak has spilled over to New Mexico and Oklahoma. In New Mexico, officials reported Friday that the case count has risen to 42 cases, with two hospitalizations and one death in an unvaccinated adult. In Oklahoma, the case count stands at four.
Measles arrives in Kansas, spreads quickly in undervaccinated counties Read More »