Troubling bird flu study suggests human cases are going undetected
Poor surveillance —
A small sample of farm workers is enough to confirm fears about H5N1 outbreak.

Tony C. French/Getty
A small study in Texas suggests that human bird flu cases are being missed on dairy farms where the H5N1 virus has taken off in cows, sparking an unprecedented nationwide outbreak.
The finding adds some data to what many experts have suspected amid the outbreak. But the authors of the study, led by researchers at the University of Texas Medical Branch in Galveston, went further, stating bluntly why the US is failing to fully surveil, let alone contain, a virus with pandemic potential.
“Due to fears that research might damage dairy businesses, studies like this one have been few,” the authors write in the topline summary of their study, which was posted online as a pre-print and had not been peer-reviewed.
The study authors, led by Gregory Gray, were invited to two undisclosed dairy farms in Texas that experienced H5N1 outbreaks in their herds starting in early and late March, respectively. The researchers had a previously approved research protocol to study novel respiratory viruses on dairy farms, easing the ability to quickly begin the work.
Rare study
“Farm A” had 7,200 cows and 180 workers. Illnesses began on March 6, and nearly 5 percent of the herd was estimated to be affected during the outbreak. “Farm B” had 8,200 cows and 45 workers. After illnesses began on March 20, an estimated 14 percent of the herd was affected.
The researchers first visited Farm A on April 3 and Farm B on April 4, collecting swabs and samples at each. Based on the previously approved protocol, they were limited to taking nasal swabs and blood samples from no more than 10 workers per farm. On Farm A, 10 workers provided nasal swabs and blood samples. On Farm B, only seven agreed to give nasal swabs, and four gave blood samples.
While swabs from cows, milk, a dead bird, and a sample of fecal slurry showed signs of H5N1, all of the nasal swabs from the 14 humans were negative. However, when researchers looked for H5N1-targeting antibodies in their blood—an indicator that they were previously infected—two of the 14, about 14 percent, were positive.
Both of the workers with previous infections, a man and a woman, were from Farm A. And both reported having flu-like symptoms. The man worked inside cattle corrals, close to the animals, and he reported having a cough at the time the samples were taken. The woman, meanwhile, worked in the cafeteria on the farm and reported recently recovering from an illness that included fever, cough, and sore throat. She noted that other people on the farm had similar respiratory illnesses around when she did.
The finding suggests human cases of H5N1 are going undetected. Moreover, managing to find evidence of two undetected infections in a sample of just 14 workers suggests it may not be hard to find more. The Centers for Disease Control and Prevention estimates that around 200,000 people work with livestock in the US.
A “compelling case”
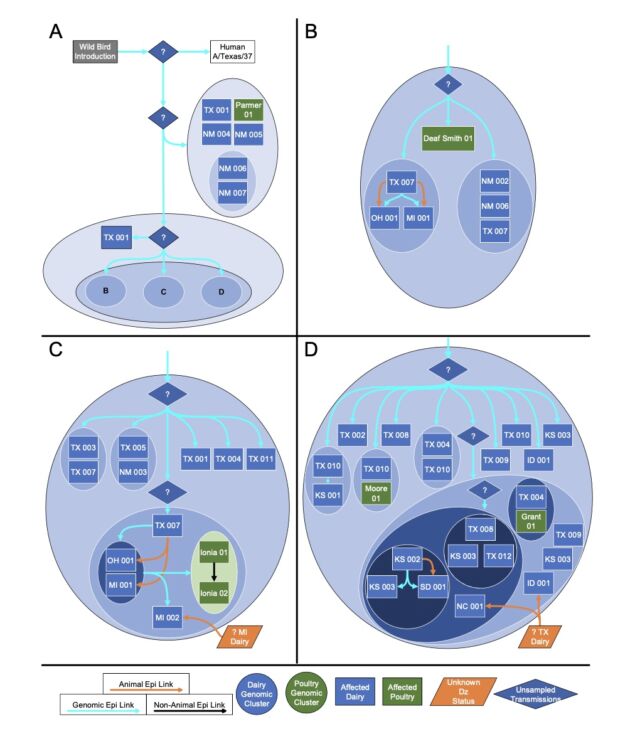
To date, the virus has infected at least 175 dairy farms in 13 states. The official tally of human cases in the dairy outbreak is 14: four in dairy farm workers and 10 in workers on poultry farms with infections linked to the dairy outbreak.
“I am very confident there are more people being infected than we know about,” Gray told KFF, which first reported on the study. “Largely, that’s because our surveillance has been so poor.”
Known infections in humans have all been mild so far. But experts are anxious that with each new infection, the wily H5N1 virus is getting new opportunities to adapt further to humans. If the virus evolves to cause more severe disease and spread from human to human, it could spark another pandemic.
Federal officials are also worried about this potential threat. In a press briefing Tuesday, Nirav Shah, the CDC’s principal deputy director, announced a $5 million effort to vaccinate farm workers—but against seasonal flu.
Shah explained that the CDC is concerned that if farm workers are infected with H5N1 and the seasonal flu at the same time, the viruses could exchange genetic segments—a process called reassortment. This could give rise to the pandemic threat experts are worried about. By vaccinating the workers against the seasonal flu, it could potentially prevent the viruses from comingling in one person, Shah suggested.
The US does have a bird flu-specific vaccine available. But in the briefing, Shah said that the use of that vaccine in farm workers is not planned for now, though there’s still active discussion on the possibility. The lack of severe disease and no documented human-to-human transmission from H5N1 infections both argue against deploying a new vaccine, Shah said. “There has to be a strong and compelling case,” he added. Shah also suggested that the agency expects vaccine uptake to be low among farm workers.
Troubling bird flu study suggests human cases are going undetected Read More »