US measles cases reach 5-year high; 15 states report cases, Texas outbreak grows
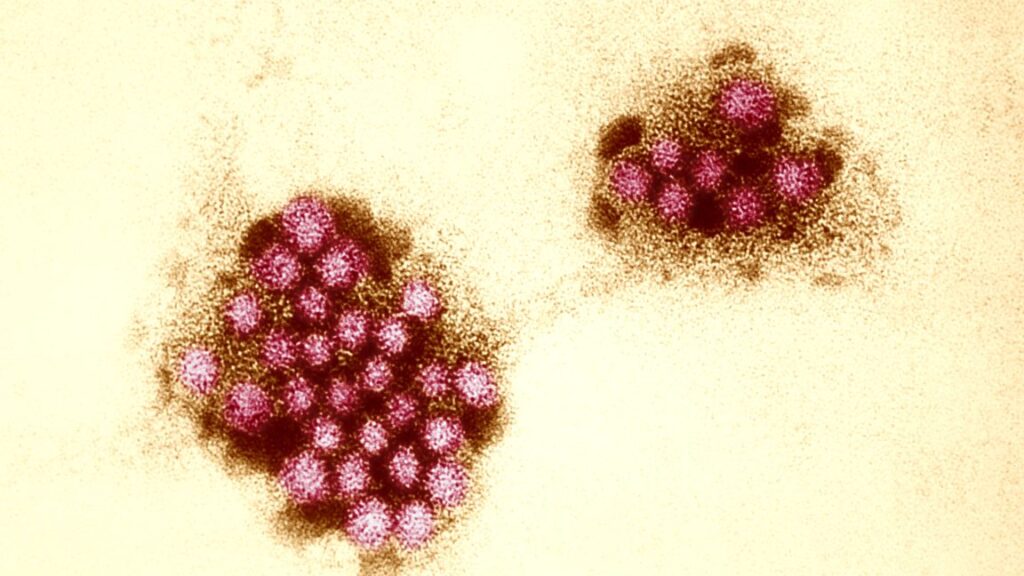
The US has now recorded over 300 measles cases just three months into 2025, exceeding the yearly case counts for all years after 2019. The bulk of this year’s cases are from an outbreak that erupted in an undervaccinated county in West Texas in late January, which has since spread to New Mexico and Oklahoma.
As of the afternoon of March 14, Texas reports 259 cases across 11 counties, 34 hospitalizations, and one death, which occurred in an unvaccinated 6-year-old girl. New Mexico reports 35 cases across two counties, two hospitalizations, and one death. That death occurred in an unvaccinated adult who did not seek medical treatment and tested positive for the virus posthumously. The cause of death is still under investigation. Oklahoma reports two probable cases linked to the outbreak.
In addition to Texas, New Mexico, and Oklahoma, 12 other states have reported at least one confirmed measles case since the start of the year: Alaska, California, Florida, Georgia, Kentucky, Maryland, New Jersey, New York, Pennsylvania, Rhode Island, Vermont, and Washington. According to the Centers for Disease Control and Prevention, this year has seen three measles outbreaks, defined as three or more related cases.
As of March 13, the CDC reported 301 confirmed cases, which do not include 36 new cases reported today in Texas and two in New Mexico.
“Measles is back”
Since 2000, when health officials victoriously declared measles eliminated from the US thanks to concerted vaccination campaigns, only three other years have had higher tallies of measles cases. In 2014, the country saw 667 measles cases. In 2018, there were 381 cases. And in 2019—when the country was on the verge of losing its elimination status—there was a startling 1,274 cases, largely driven by massive outbreaks in New York. Measles is considered eliminated if there is no continuous spread in the country over the course of at least 12 months. (This is not to be confused with “eradication,” which is defined as “permanent reduction to zero of the worldwide incidence” of an infectious disease. Smallpox and rinderpest are the only pathogens humans have eradicated.)
US measles cases reach 5-year high; 15 states report cases, Texas outbreak grows Read More »