This flu season looks grim as H3N2 emerges with mutations
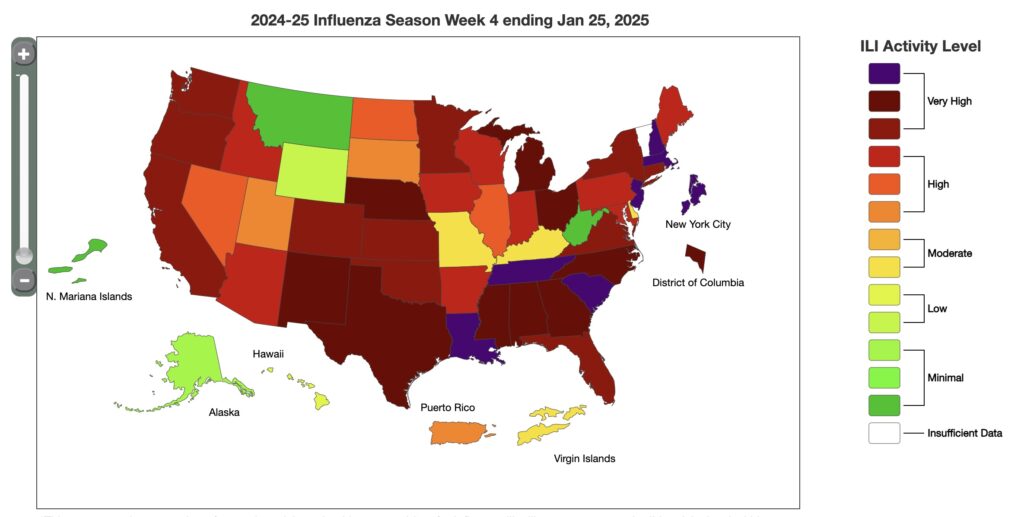
Health officials in the United Kingdom are warning that this year’s flu season for the Northern Hemisphere is looking like it will be particularly rough—and the US is not prepared.
The bleak outlook is driven by a new strain of H3N2, which emerged over the summer (at the end of the Southern Hemisphere’s season) sporting several mutations. Those changes are not enough to spark the direst of circumstances—a deadly pandemic—but they could help the virus dodge immune responses, resulting in an outsized number of severe illnesses that could put a significant strain on hospitals and clinics.
In the UK, the virus has taken off. The region’s flu season has started around five weeks earlier than normal and is making a swift ascent.
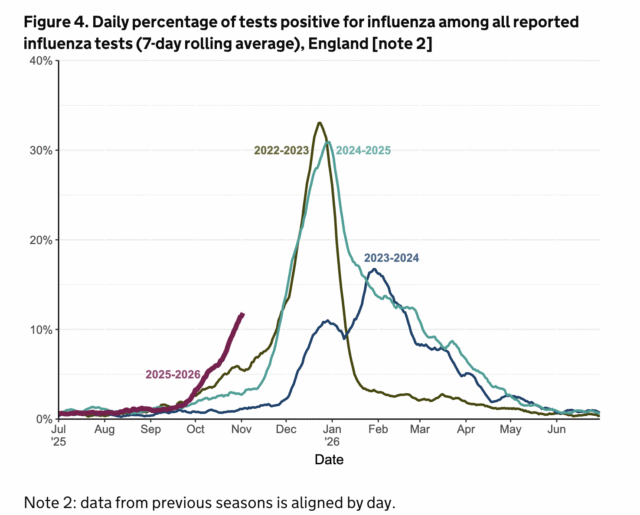
The UK’s flu season progress. Credit: UKHSA
Jim Mackey, who became chief executive of NHS England in April, is bracing for influenza’s wrath. “There’s no doubt this winter will be one of the toughest our staff have ever faced,” Mackey told The BMJ. “Since stepping into this role, the thought of a long, drawn-out flu season has kept me awake at night. And, unfortunately, it looks like that fear is becoming reality.”
Almost all of the UK cases so far this year have been from influenza A strains, with H3N2 accounting for the lion’s share, according to the UK Health Security Agency. The two circulating influenza A strains are the new H3N2 strain and an H1N1 strain, with an influenza B strain circulating at very low rates. In the latest UK data, H3N2 was behind over 90 percent of cases that had their influenza virus type analyzed.
“Of the two seasonal influenza A viruses, the current dominant circulating virus (A/H3N2) tends to cause more severe illness than A/H1N1, particularly in older adults,” Antonia Ho, an infectious diseases expert at the University of Glasgow, said in a statement. And the early start of the flu season only makes things worse, since not as many people are vaccinated early on, Ho added. “From previous experience, influenza waves that start early tend to affect a larger number of people in the population.”
This flu season looks grim as H3N2 emerges with mutations Read More »