Pixel Watch 3 gets FDA approval to alert you if you’re dying
Google released the Pixel Watch 3 last fall alongside the Pixel 9 family, sporting the same curvy look as the last two versions. The Pixel Watch 3 came with a new feature called Loss of Pulse Detection, which can detect impending death due to a stopped heart. Google wasn’t allowed to unlock that feature in the US until it got regulatory approval, but the Food and Drug Administration has finally given Google the go-ahead to activate Loss of Pulse Detection.
Numerous smartwatches can use health sensors to monitor for sudden health events. For example, the Pixel Watch, Apple Watch, and others can detect atrial fibrillation (AFib), a type of irregular heartbeat that could indicate an impending stroke or heart attack. Google claims Loss of Pulse Detection goes further, offering new functionality on a consumer wearable.
Like the EKG features that became standard a few years back, Loss of Pulse Detection requires regulatory approval. Google was able to get clearance to ship the Pixel Watch 3 with Loss of Pulse Detection in a few European countries, eventually expanding to 14 nations: Austria, Belgium, Denmark, France, Germany, Ireland, Italy, Netherlands, Norway, Portugal, Spain, Sweden, Switzerland, and the United Kingdom. It noted at the time more countries would get access as regulators approved the feature, and the FDA was apparently the first to come through outside of Europe, boosting support to 15 countries.
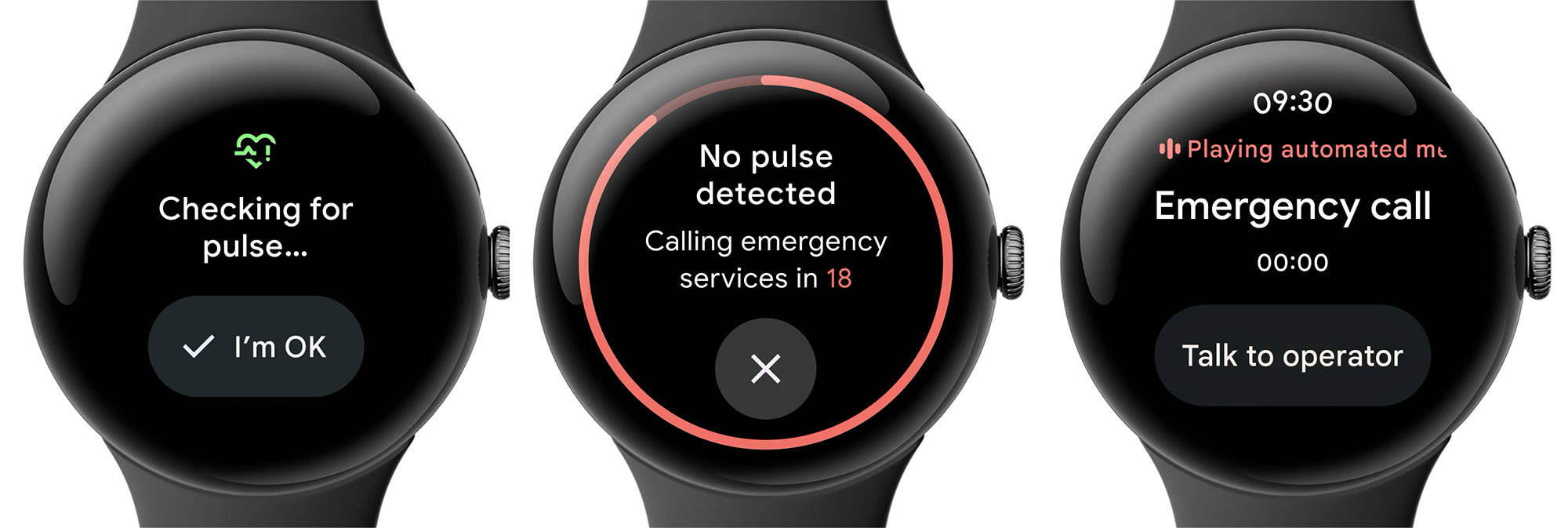
Credit: Google
The Pixel Watch 3 doesn’t include any new or unique sensors to power Loss of Pulse Detection—it’s just using the sensors common to smartwatches in slightly different ways. The watch uses a “multi-path” heart rate sensor that is capable of taking readings once per second. When the sensor no longer detects a pulse, that usually means you’ve taken the watch off. It’s quick to make that determination, locking the watch in about a second. That’s great for security but a little annoying if you were readjusting it on your wrist.
Pixel Watch 3 gets FDA approval to alert you if you’re dying Read More »