Trump admin. fires USDA staff working on bird flu, immediately backpedals
Over the weekend, the Trump administration fired several frontline responders to the ongoing H5N1 bird flu outbreak—then quickly backpedaled, rescinding those terminations and attempting to reinstate the critical staff.
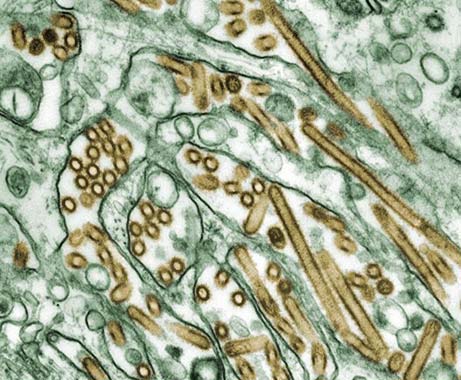
The termination letters went out to employees at the US Department of Agriculture, one of the agencies leading the federal response to the outbreak that continues to plague US dairy farms and ravage poultry operations, affecting over 160 million birds and sending egg prices soaring. As the virus continues to spread, infectious disease experts fear it could evolve to spread among humans and cause more severe disease. So far, the Centers for Disease Control and Prevention has documented 68 cases in humans, one of which was fatal.
Prior to Trump taking office, health experts had criticized the country’s response to H5N1 for lack of transparency at times, sluggishness, inadequate testing, and its inability to halt transmission among dairy farms, which was once considered containable. To date, 972 herds across 17 states have been infected since last March, including 36 herds in the last 30 days.
In a statement to Ars Technica, a USDA spokesperson said that the agency views the response to the outbreak of H5N1—a highly pathogenic avian influenza (HPAI)—as a priority. As such, the agency had protected some positions from staff cuts by granting exemptions, which went to veterinarians, animal health technicians, and others. But not all were exempted, and some were fired.
“Although several positions supporting HPAI were notified of their terminations over the weekend, we are working to swiftly rectify the situation and rescind those letters,” the spokesperson said.
The USDA did not respond to Ars Technica’s questions regarding how many employees working on the outbreak were fired, how many of those terminations were rescinded, or how many employees have been reinstated since the weekend.
The cuts are part of a larger, brutal effort by the Trump administration to slash federal agencies, and the cuts have imperiled other critical government and public services. In recent days, several agencies, including the National Institutes of Health, the CDC, the National Science Foundation, and the Department of Energy, among others, have been gutted. At CDC, cuts devastated the agency’s premier disease detectives program—the Epidemic Intelligence Service—members of which are critical to responding to outbreaks and other health emergencies.
Trump admin. fires USDA staff working on bird flu, immediately backpedals Read More »