Trump health official ousted after allegedly giving himself a fake title
Steven Hatfill, a senior advisor for the Department of Health and Human Services was fired over the weekend, with health officials telling reporters that he was terminated for giving himself a fake, inflated title and for not cooperating with leadership.
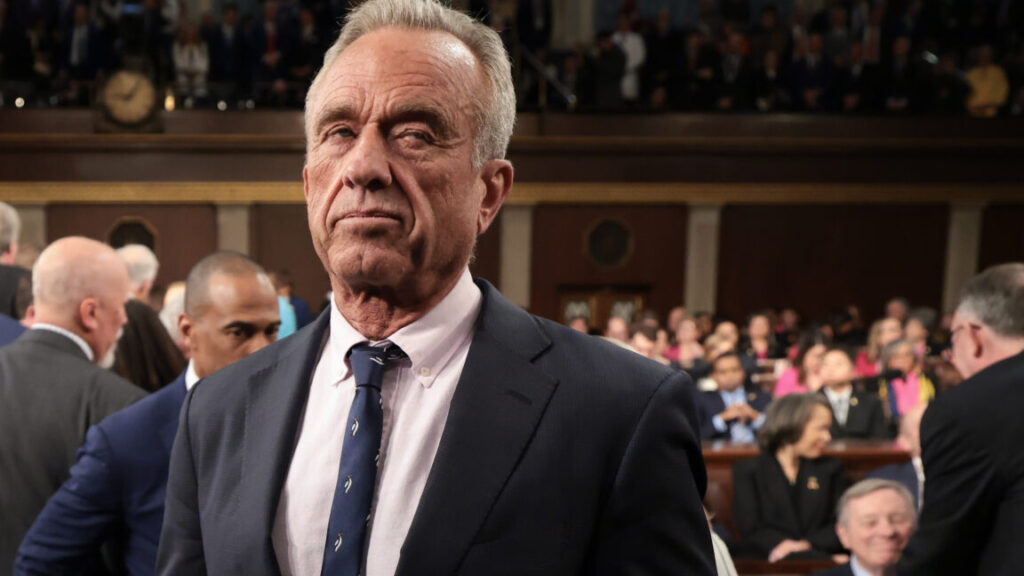
For his part, Hatfill told The New York Times that his ouster was part of “a coup to overthrow M. Kennedy,” referring to anti-vaccine Health Secretary Robert F. Kennedy Jr. Further, Hatfill said the coup was being orchestrated by Matt Buckham, Kennedy’s chief of staff, though Hatfill didn’t provide any explanation of how his ouster was evidence of that. An HHS spokesperson responded to the allegation, telling the Times that “firing a staff member for cause does not add up to a coup.”
Bloomberg was first to report Hatfill’s termination.
Background
While Hatfill was not a particularly prominent member of the Trump administration, his role—and now ouster—is notable for several reasons. Most recently, he was seen as a driving force in Kennedy’s decision to cancel $500 million in federal grants for developing mRNA vaccines against future pandemic threats. The medical and scientific communities sharply criticized the cancellations, saying they leave the country ill-prepared for the next pandemic and create a void for China or other countries to lead in scientific advances. Still, Hatfill is especially hostile to mRNA vaccine technology. In an appearance on Steve Bannon’s show in August, Hatfill falsely claimed that mRNA COVID-19 vaccines cause “biochemical havoc” on cells.
Rather than support life-saving vaccines, Hatfill embraces ineffective treatments for COVID-19, including the anti-malarial drug hydroxychloroquine and the de-worming drug ivermectin. He touted those ineffective treatments during the height of the pandemic, when he was a White House advisor during Trump’s first term.
But Hatfill might best be known for being wrongly accused of carrying out the 2001 anthrax attacks that killed five people and sickened 17. The attacks involved a strain of anthrax that was used at the United States Army Medical Research Institute of Infectious Diseases (USAMRIID), where Hatfill had a fellowship from 1997 to 1999—though he worked on viruses while there, not bacterial diseases like anthrax. The FBI publicly announced Hatfill as a person of interest in the case in 2002. Hatfill filed a lawsuit against the Department of Justice over privacy violations, which the department settled in 2008, paying Hatfill $5.8 million. The FBI went on to accuse Bruce Ivins, another USAMRIID scientist, of carrying out the attacks. But, Ivins died by suicide in 2008 before being charged and doubts remain about the case against him.
Trump health official ousted after allegedly giving himself a fake title Read More »