CDC tormented: HR workers summoned from furlough to lay off themselves, others
Traumatized CDC has lost 33% of its workforce this year, union says.
ATLANTA, GEORGIA – AUGUST 9: Bullet holes are seen in windows at the Centers For Disease Control (CDC) Global Headquarters following a shooting that left two dead, on August 9, 2025 in Atlanta, Georgia. On August 8, a gunman opened fire near the headquarters of the Centers for Disease Control, killing a DeKalb County Police Department officer before being found dead by gunfire. Credit: Getty | Elijah Nouvelage
The dust is still settling at the Centers for Disease Control and Prevention after a mass layoff on Friday, which former employees at the beleaguered agency are describing as a massacre.
In separate press briefings on Tuesday, a network of terminated CDC staff that goes by the name the National Public Health Coalition, and the union representing employees at the agency discussed what the wide-scale cuts mean for the American people, as well as the trauma, despair, and damage they have wreaked on the workers of the once-premier public health agency.
In a normal federal layoff—called a reduction in force, or RIF—the agency would be given a full outline of the roles and branches or divisions affected, as well as some explanation for the cuts, such as alleged fraud, abuse, or redundancy. However, the Trump administration has provided no such information or explanation, leaving current and former employees to essentially crowdsource what has been lost and only guess at the possible reasons.
The numbers
The union representing CDC workers, the American Federation of Government Employees (AFGE) Local 2883, has been assessing the cuts since termination emails began arriving in employee inboxes late Friday. The union estimates that the Trump administration sent termination notices to 1,300 CDC employees on Friday, in what they called an illegal “politically-motivated stunt.” Of those 1,300 terminations, around 700 were rescinded, beginning on Saturday.
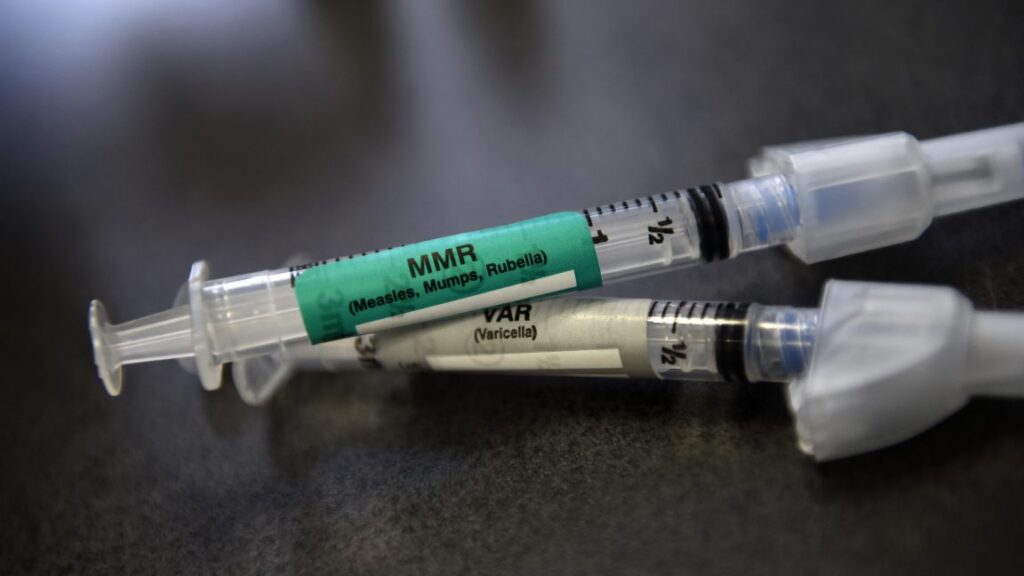
The Trump administration said the 700 rescinded terminations were sent due to a “coding error.” But CDC workers didn’t buy that explanation, saying all the terminations were intentional, and some were only reversed after backlash erupted when people realized what the administration was trying to cut—for example, terminating the experts responding to domestic measles outbreaks and those responding to an Ebola outbreak in the Democratic Republic of the Congo who received RIF notices that were later rescinded. Still, with the rescissions, some 600 terminations appear to remain.
In all, the union estimated that the CDC has lost 33 percent of its workforce since the start of the Trump administration. In January, there were roughly 13,000 CDC workers total. Since then, about 3,000 have been fully separated from the agency, including 600 laid off in a RIF on April 1, and 2,400 who were either fired or forced out amid pressure campaigns. An additional 1,300 have been laid off but are not yet fully separated from the agency; they remain on paid administrative leave but are unable to do their work.
In the RIF Friday, laid-off employees said they were given notices that list their termination effective date as December 8, leaving a 60-day period in which they would be on administrative leave.
The RIF was carried out amid an ongoing government shutdown over a health care funding dispute, and the Trump administration has claimed that the RIF is a consequence of the shutdown. But the union, along with federal employment lawyers and even some senior government officials, say a RIF during a shutdown is illegal; a temporary lapse in government funding is not a legitimate reason for a RIF under federal regulations, and it runs afoul of a federal law that prohibits the government from incurring new costs during a shutdown, such as by promising severance packages.
Brutal cuts
In practice, a RIF amid a shutdown added more trauma to the demoralized staff. In opening remarks, Local AFGE 2883 President Yolanda Jacobs noted that the CDC Human Resources staff had been furloughed during the shutdown but were temporarily brought back into work just so they could process termination letters—including their own. A terminated CDC employee who spoke on condition of anonymity said that more than 90 percent of the HR staff is now gone.
Among the terminations were also mental health workers who were helping CDC staff recover from an August attack, in which a gunman fired over 500 rounds at CDC buildings full of agency employees and killed a local police officer.
Another terminated CDC worker who spoke on the condition of anonymity discussed the personal toll of the RIF. She had worked at the agency for over two decades and learned of her termination Friday night as she was doing dishes after making homemade pizza with her family—money worries kept them from ordering out. Her phone “started going crazy” as coworkers were checking in after receiving their RIF notices. She dug out her work laptop, which had been set aside since she was furloughed, to find her own RIF notice at the top of her inbox.
As text messages continued to come in through the night, she said it was “heartbreaking and devastating” when she realized the Trump administration was “actually dismantling us.”
“These are just hardworking Americans who just want to do their job, who just want to help people, who want to make sure the correct information is out there [and] that we are preventing things from happening,” she said.
Since the RIF has sunk in, she has started to worry more for her family and their finances. During the furlough, paychecks are uncertain. And her effective termination date in December will land between holidays, when hiring is slow. She worried about affording Christmas presents for her family.
She also said that staff have asked about getting other jobs while on administrative leave but were told that in order to do that, they would need to get approval from the CDC’s ethics office to ensure there were no conflicts of interest. But staff can’t actually do that because everyone at the ethics office also got RIF notices.
Losses
Throughout the briefings yesterday, staff highlighted that the RIF did not just trim here and there, as one might expect with cuts designed to make the organization leaner. Instead, it lopped off entire teams and branches, completely shutting down whole lines of work.
One former CDC employee spoke broadly of big hits to experts in chronic disease, global health, and the National Center for Health Statistics, which runs critical data collection that states and local health departments rely on. The CDC’s library staff are all gone. Suicide prevention experts have been cut, as well as communications and policy staff, who develop briefings and provide information to Congress members.
Abigail Tighe, a former CDC employee with National Public Health Coalition, tried to put the cuts in context, saying: “We are losing the people with all the knowledge to prevent childhood drownings, child abuse, and suicide. We’re losing the experts who help us track and understand the health and safety needs of our communities [and] the brave and brilliant professionals who, on a moment’s notice, respond to new and unknown outbreaks across the world. And that’s just a few examples.”
A terminated scientist who spoke on condition of anonymity said that her entire office was eliminated in the RIF. “My heart breaks for my colleagues and friends who have been tormented, traumatized, shot at, threatened daily. These are kind, hardworking, thoughtful people whose lives are being overturned,” she said.
But, “ultimately,” she said, “I am terrified for the public safety of our country.”
Beth is Ars Technica’s Senior Health Reporter. Beth has a Ph.D. in microbiology from the University of North Carolina at Chapel Hill and attended the Science Communication program at the University of California, Santa Cruz. She specializes in covering infectious diseases, public health, and microbes.
CDC tormented: HR workers summoned from furlough to lay off themselves, others Read More »