retracted —
A large number of other, non-retracted studies find mifepristone to be very safe.
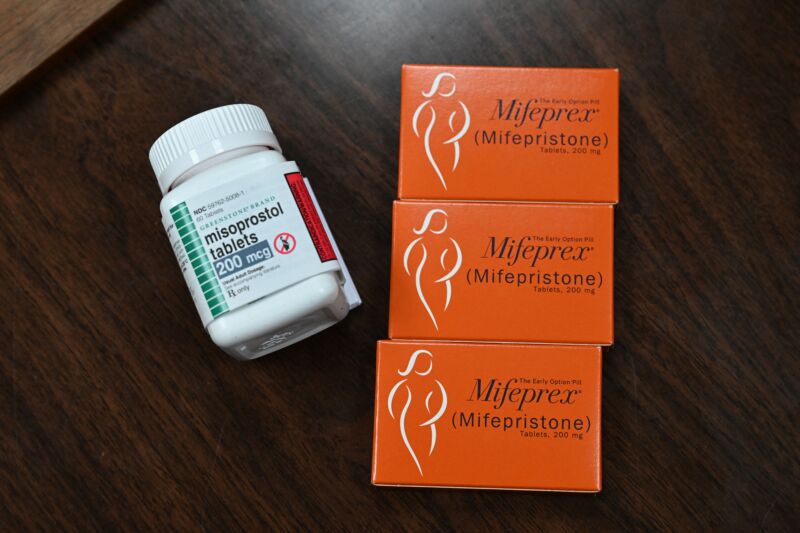
Enlarge / Mifepristone (Mifeprex) and misoprostol, the two drugs used in a medication abortion, are seen at the Women’s Reproductive Clinic, which provides legal medication abortion services, in Santa Teresa, New Mexico, on June 17, 2022.
Scientific journal publisher Sage has retracted key abortion studies cited by anti-abortion groups in a legal case aiming to revoke regulatory approval of the abortion and miscarriage medication, mifepristone—a case that has reached the US Supreme Court, with a hearing scheduled for March 26.
On Monday, Sage announced the retraction of three studies, all published in the journal Health Services Research and Managerial Epidemiology. All three were led by James Studnicki, who works for The Charlotte Lozier Institute, a research arm of Susan B. Anthony Pro-Life America. The publisher said the retractions were based on various problems related to the studies’ methods, analyses, and presentation, as well as undisclosed conflicts of interest.
Two of the studies were cited by anti-abortion groups in their lawsuit against the Food and Drug Administration (Alliance for Hippocratic Medicine v. FDA), which claimed the regulator’s approval and regulation of mifepristone was unlawful. The two studies were also cited by District Judge Matthew Kacsmaryk in Texas, who issued a preliminary injunction last April to revoke the FDA’s 2000 approval of mifepristone. A conservative panel of judges for the 5th Circuit Court of Appeals in New Orleans partially reversed that ruling months later, but the Supreme Court froze the lower court’s order until the appeals process had concluded.
Mifepristone, considered safe and effective by the FDA and medical experts, is used in over half of abortions in the US.
Criticism
Amid the legal dispute, the now-retracted studies drew immediate criticism from experts, who pointed out flaws. Of the three, the most influential and heavily criticized is the 2021 study titled “A Longitudinal Cohort Study of Emergency Room Utilization Following Mifepristone Chemical and Surgical Abortions, 1999–2015” (PDF). The study suggested that up to 35 percent of women on Medicaid who had a medication abortion between 2001 and 2015 visited an emergency department within 30 days afterward. Its main claim was that medication abortions led to a higher rate of emergency department visits than surgical abortions.
Critics noted a number of problems: The study looked at all emergency department visits, not only visits related to abortion. This could capture medical care beyond abortion-related conditions, because people on Medicaid often lack primary care and resort to going to emergency departments for routine care. When the researchers tried to narrow down the visits to just those related to abortion, they included medical codes that were not related to abortion, such as codes for ectopic pregnancy, and they didn’t capture the seriousness of the condition that prompted the visit. Medication abortions can cause bleeding, and women can go to the emergency department if they don’t know what amount of bleeding is normal. The study also counted multiple visits from the same individual patient as multiple visits, likely inflating the numbers. Last, the study did not put the data in context of emergency department use by Medicaid beneficiaries in general over the time period.
In contrast to Studnicki’s study, the American College of Obstetricians and Gynecologists notes that studies looking at tens of thousands of medication abortions have concluded that “Serious side effects occur in less than 1 percent of patients, and major adverse events—significant infection, blood loss, or hospitalization—occur in less than 0.3 percent of patients. The risk of death is almost non-existent.”